Minor Tooth Movement: Overview
One of the most versatile techniques in dentistry today is the application of Minor Tooth Movement (MTM®). This treatment option comprises movement of teeth using plastic aligners and thermopliers (Dentsply Raintree Essix®, Dentsply, Sarasota, Florida) and produces outstanding aesthetics and function. This method is a minimally invasive approach to patient care.
Technically speaking, MTM involves the movement of 1-4 teeth per arch using continuous, gentle force. Traditional orthodontic movements, consisting of rotation, tipping, and lateral position change, can be achieved by the patient wearing an in-office fabricated aligner. At each return patient visit, gentle pressure is applied to the aligner, using thermopliers that are designed to create intentional, guided force of up to 1 mm per month, resulting in correct alignment. Most cases treated by this method are completed in 6 months or less.
Case Selection for MTM
Case selection is paramount to meet the parameters of MTM. MTM can be used to treat easy orthodontic cases, refine previous alignments, and set the stage for restorative and esthetic cases that may involve composite bonding, crowns, veneers, or implants. Any patient under consideration for MTM should have permanent dentition, present with a healthy periodontal state, have no temporomandibular joint symptoms, and demonstrate adequate arch length. Criteria that warn practitioners of poor case selection are severe incisor rotation, xerostomia, active caries, and a non-compliant patient.
A key component in many minor tooth movement cases is the available arch space in which to re-align the teeth. Length discrepancies must be considered for a successful treatment outcome. Arch presentations that exceed 2 mm in length discrepancy are not considered within the guiding principles of MTM case selection, and are not acceptable cases for this method of treatment. Dentists must make sure to accurately measure the widest dimension of each tooth, from canine to canine. Each of these widths are then added together to arrive at the total width for the teeth present within the arch. This measurement is compared to the measurement of the existing arch from the distal to distal of each canine. The difference of these 2 values — given arch length and total teeth width value –translates to the amount of space required to complete alignment.
Techniques for MTM
Symmetry and Staging
Once a determination is made that a case qualifies for MTM, the next level of treatment consideration concerns symmetry and staging or sequencing. Most of the time, teeth will not be identical in size, therefore they are “disproportional.” These disproportions can be used to the clinician’s advantage to identify surfaces, if reduced, that may promote or create a more symmetrical appearance. These reductions are the compensation required to align the teeth within the current arch.
To gain arch space, the clinician can procline the teeth — if the opposing arch allows or use interproximal reduction (IPR). Interproximal reduction is the technique used to create interproximal space so that teeth within the arch can pass each other into alignment without colliding. Random tooth reduction is not recommended for MTM. Rather, carefully planned and staged tooth reduction or contouring is a much better approach to guarantee not only patient acceptance, but also case success. Done correctly, IPR should not be painful, should always allow adequate remaining tooth structure that is not sensitive, and should respect the initial tooth anatomy to provide pleasing final esthetics. I recommend performing IPR using a safe-tipped diamond burr, smoothing the affected surfaces with finishing strips, and measuring with the appropriate interproximal gauge.
Model Preparation
Model preparation is also critical to MTM success. Correctly positioned teeth require 2 components — force on one side and block-out (the space that the tooth will move into) on the other. This element is central to MTM. Block-out material can consist of composite or Triad material. Because these models will undergo a thermoforming or vacuum-forming process, wax should not to be used because it will melt and not allow the proper amount of space necessary for correct tooth repositioning.
To create the aligner, specific tooth-moving plastic with innate properties that remain and stay constant during the treatment is selected. I predominately use either ACE or C+ plastic (Dentsply, Raintree Essix, Sarasota, Florida) for all cases. Model preparation consists of spraying the model with a separator, then thermoforming or vacuum-forming the plastic over the model to create the aligner. The aligner is finalized by carefully separating the plastic from the model, followed by trimming and polishing (Figure 1).

Figure 1. MTM clear aligner.
The final component of movement is force. This is achieved by the use of thermopliers that place directional forces on the desired teeth to be moved. (Figure 2).

Figure 2. Mandibular thermoplier.
Each plier is properly gauged to determine the amount of force (eg, usually 0.5 mm); heated according to the plastic being used; and then activated by squeezing a force bump into the aligner. As a result of the properties of the plastic material, the plastic undergoes a thermochange process, so when the force bump cools, the plastic will remain in that desired position and will not change or minimize. If heat is not used, the plastic will stretch, rebound, and collapse — thus, the intentional force bump will lessen and not be effective.
First Case: Crooked Lower Teeth
A 26-year old patient presented with good oral hygiene, no existing restorations, and no caries. Her chief concern was that her “2 front lower teeth were crooked.” She went on to explain that she had orthodontic treatment as a teenager and did not wear her retainers as prescribed (Figure 3).

Figure 3. Mandibular arch pre-treatment.
A hybrid polyvinyl impression was taken of both arches to create working and study models. A standard series of photographs was taken and loaded into a orthodontic template. Measurements were made on the study model to determine arch length discrepancy. The patient presented with a need for 1.5 mm of space. This patient was deemed an excellent candidate for MTM treatment.
On the working model, block-out composite was placed on the distal-facial aspects of both teeth # 24 and #25. Once completed, the block-out appeared to create a “final wax-up” appearance, repositioning the teeth completely. ACE plastic was selected to thermoform over the model using a thermoforming machine. The fabricated aligner was removed from the model, trimmed, and polished.
At the patient’s first MTM appointment, the aligner was delivered to confirm its fit. Translating from the study model, IPR was to be performed on the distal interproximal surfaces on teeth #24 and #25. A safe-tipped diamond burr was used to perform 0.5 mm of interproximal reduction on the distal surfaces of the mandibular central incisors. A finishing strip was used to smooth the treated surface. Finally, floss was used to confirm the final surface smoothness, free of any ledges. The mandibular thermoplier was selected to create a force bump on the distal lingual aspect of on teeth #24 and #25. The aligner was delivered and the patient was given instructions on wear and care of the aligner and was scheduled to be seen 1 month later.
At the next appointment, the original aligner was ultrasonically cleaned and confirmed for fit. The same thermoplier used initially to create the force bump was used again. Force bumps of 0.5 mm were placed on the distal-lingual surfaces, directionally forcing the teeth to align facially. The patient was to return in 1 month.
The patient presented at her third appointment with properly aligned teeth. She was extremely pleased with her result. A final alginate impression was taken to create a maintainer that she was very motivated to wear (Figure 4).

Figure 4. Mandibular arch final treatment.
Second Case: Rotated Maxillary Laterals
This 35-year-old patient was concerned that her front teeth were wearing at an angle (Figure 5).

Figure 5. Full smile pre-treatment.
Closer examination revealed that because of the distal rotation of both maxillary laterals (teeth #7 and #10), her occluding mandibular canines were interfering with the maxillary lateral incisal edges in excursions (Figure 6).

Figure 6. Maxillary arch pre-treatment.
The patient’s slight distally rotated tooth #26 also needed alignment (Figure 7).

Figure 7. Mandibular arch pre-treatment.
Consideration of treatment options needed to respect both function and esthetics to provide the proper long-term outcome. To place composite or veneers on these teeth without proper tooth repositioning would have certainly caused failure due to the patient’s lack of canine guidance. The correct approach for this case was a combination of aligning the teeth with MTM and then restoring the maxillary laterals with composite.
Final impressions were made of both arches using polyvinyl impression material. A technique similar to a final wax-up was made to use as a mock-up model to place block-out material (flowable composite, in this case). This also acted as a guide for the directional forces to be placed on the teeth requiring repositioning. Care was made not to use wax as the block-out material because it would melt during the thermoforming procedure. The aligner was thermoformed over the finalized model, and then trimmed and polished.
Movement was initiated by placing intentional forces on the maxillary canines to rotate them in a mesial-labial direction. Aligners are recommended to be worn for 22 hours a day, 7 days a week. During this time, the alignment of tooth #26 was also corrected. Each directional force was created by heating the thermoplier, then dimpling the aligner plastic where the intended movement was to follow. The patient was engaged in active monthly treatment for 4 months. Her final alignment is shown in both the maxillary and mandibular arches (Figures 8, 9).

Figure 8. Maxillary arch final.

Figure 9. Mandibular final treatment.
The patient opted for composite bonding to restore her maxillary laterals using a microhybrid composite. Teeth #7 and #10 were restored using a total-etch and bond system to maximize enamel adhesion. The patient was very pleased with her improved esthetics and function (Figure 10).

Figure 10. Final alignment with composite bonding
Third Case: A Crossbite
A 42-year-old patient had been consistent with recare visits and had previously been told by another practitioner that she should undergo minor orthodontic treatment. The patient was adamant that traditional brackets and wires were not a treatment consideration. Clear aligners were a more acceptable option (Figure 11).

Figure 11. Pre-treatmentview.
Polyvinyl impressions were taken to create both working and study models. In this particular case, after measuring the arch length, no discrepancy was found, therefore the case was ideal for MTM and could proceed without any IPR (Figures 12, 13).
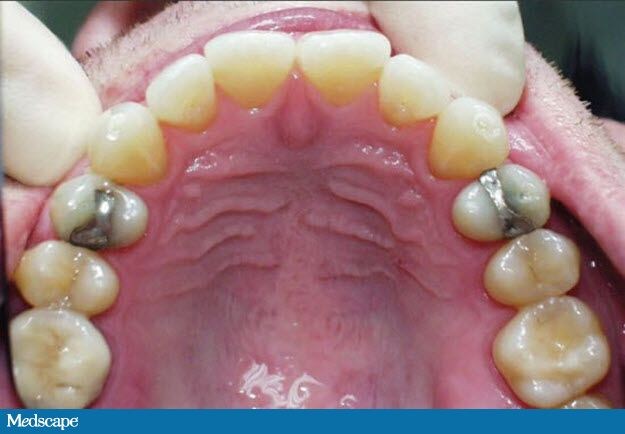
Figure 12. Maxillary arch pre-treatment.

Figure 13. Mandibular pre-treatment.
Composite material was used as block-out and placed on specific maxillary and mandibular teeth that were to be involved or repositioned. This creation of space is critical to allow for the acceptance of the guiding force that directs each tooth into its newly anticipated position or interproximal space.
The treatment goals considered for this cases were to correct the crossbite on tooth #7, to rotate the mandibular canines into a more supportive and upright position, to round both arches, and finally, to close the black triangle between teeth #23 and #24.
ACE plastic was thermoformed over the trimmed stone and blocked-out cast. Once the plastic finished thermoforming, the rough aligner was removed, trimmed and polished.
As treatment began, directional forces were placed in the plastic aligner using specific heated thermopliersat each visit. The patient was seen monthly for 4 months to complete the esthetic/orthodontic phase (Figures 14-16).

Figure 14. Final treatment.

Figure 15. Maxillary arch final treatment.

Figure 16. Mandibular arch final treatment.
A Win-Win Dental Solution
Learning about minor tooth movement can be professionally satisfying as well as very beneficial for patient care. Patients now have the treatment option that orthodontically corrects 1-4 teeth by focusing forces placed in plastic. Earlier schools of thought would have mandated traditional wires and brackets to correctly align the malposed teeth. However, with current technology and improved plastic materials, the ability to offer MTM to patients creates a win-win for oral hygiene reasons and esthetics, thus patient compliance is excellent and well-received.
